Dr Ben Schwarz
ORTHOPAEDIC SURGEON, EAST SYDNEY PRIVATE HOSPITAL
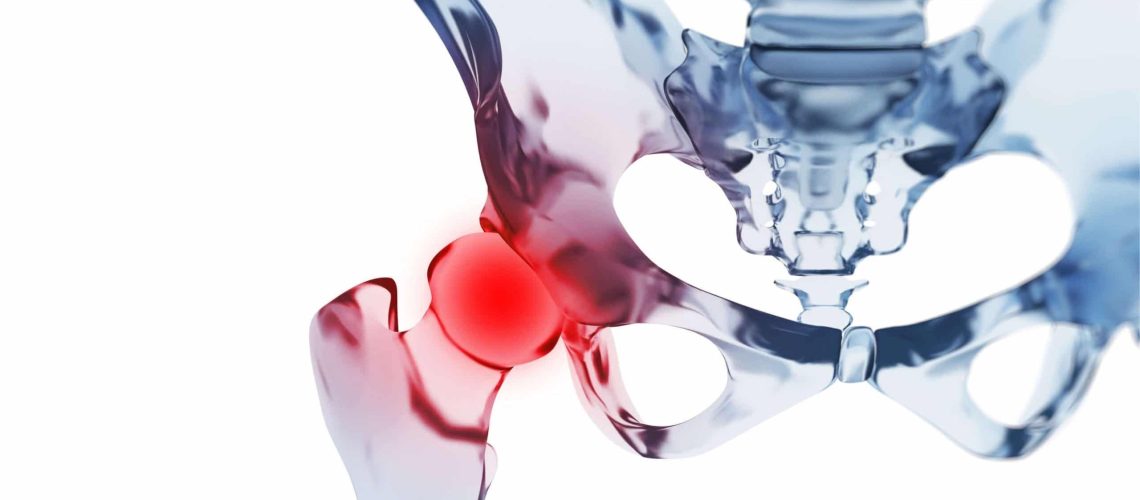
What is OsteoArthritis?
- Osteoarthritis is one of the leading causes of hip pain
- Osteoarthritis, the most common form of arthritis affecting the hip, is a chronic degenerative condition where the cartilage covering the bone ends in the joint breaks down and wears away, causing the bones to rub together
- An estimated 2.2 million (9.3%) Australians report having arthritis, according to the latest Australian National Health Survey
- Osteoarthritis can affect people of all ages, but the prevalence increases sharply from the age of 45, and affects women more than men
- Typically, arthritis is a progressive disease, meaning that it starts gradually and continues to deteriorate with time
- In Australia, compared to those without the condition, people with osteoarthritis are:
– 2.7 times as likely to report poor health
– 3.5 times as likely to report very high levels of psychological distress
– 2.8 times as likely to report severe and very severe pain.
What causes Hip OsteoArthritis?
Osteoarthritis has no specific cause, however several factors contribute to the onset and progression including:
- Female gender
- Genetic factors
- Excess weight
- Joint malalignment or abnormal shape
- Joint injury or trauma (such as dislocation or fracture)
- Repetitive joint-loading tasks (for example, kneeling, squatting and heavy lifting)
What are the symptoms of Hip OsteoArthritis?
The symptoms vary from person to person:
- Typical symptoms include pain (hip, groin, buttock or thigh pain that can radiate to the knee), and stiffness along with physical limitations due to impaired mobility
- The pain may be felt as felt as sharp, stabbing pain or a dull, burning ache
- It is most often worse with activity or after long periods of inactivity
- The pain and stiffness may interfere with everyday activities including walking, putting on shoes and socks, going up and down stairs, getting into and out of low chairs, using a car or public transport or keeping up with your grandchildren
- As symptoms progress, a limp may become noticeable, or the symptoms may occur at rest or at night
- People with osteoarthritis can experience anxiety, depression and other mental health issues
How is Hip OsteoArthritis treated?
At present, there is no cure for osteoarthritis and the disease is long-term and progressive. Treatment for osteoarthritis aims to manage symptoms, increase mobility and maximise quality of life. General practitioners (GPs) are usually the first point of contact with the health care system for people with osteoarthritis and are ideally placed to play the role of care coordinator to ensure treatment continuity.
Non-Operative treatment options for osteoarthritis include:
- Activity modification – minimising activities that exacerbate the symptoms, such as climbing stairs or high-impact exercise (e.g. running), may ease the pain and slow the worsening of symptoms
- Physical activity – exercise is an important and effective component in both the management and prevention of osteoarthritis. Exercise may help to improve symptoms and quality of life by maintaining and increasing joint flexibility, strengthening muscles around the hip, assisting in weight control and reducing the risk of other chronic diseases. Ideal low-impact activities include walking, cycling and water exercise/hydrotherapy
- Weight management – maintaining an ideal weight or losing excess weight has a significant role in reducing the symptoms of osteoarthritis and delaying the progression of the disease. Weight loss does reduce the amount of stress going through the damaged hip joint which may lead to less pain and improved mobility
- Medication – simple pain medication (such as paracetamol/panadol) or Non-Steroidal Anti-Inflammatory Drugs (such as ibuprofen/nurofen, mobic or celebrex) are often the first line used when the pain and discomfort worsens, interferes with activities of daily living or prevents a good night’s sleep. The Royal Australian College of General Practitioners strongly recommends against using opioids for the treatment of osteoarthritis, but they may be necessary in certain situations
- Platelet-Rich Plasma (PRP) and stem cells – at this time, there is not enough high-quality evidence to recommend their use. Ongoing scientific trials are underway to assess whether these have any role in hip osteoarthritis
Joint replacement surgery:
- A total hip replacement is usually very good at relieving pain, restoring joint function and improving the quality of life for people with hip osteoarthritis
- Consideration of joint replacement surgery should occur for patients with moderate-severe osteoarthritis when all appropriate non-operative options, delivered for a reasonable period of time, have failed
- The hallmarks of severe/end-stage osteoarthritis include significant joint pain, swelling and deformity, which disrupts normal sleep patterns, causes a marked reduction in walking distance and noticeable restriction of activities of daily living (such as rising from a chair or toilet seat, difficulty with climbing stairs, or putting on shoes and socks)